Research Snapshot: Can a mental health intervention help people in humanitarian settings manage chronic diseases?
Mental health symptoms experienced alongside chronic non-communicable diseases (NCDs) like diabetes and hypertension can make it difficult for patients to adhere to prescribed medication and lifestyle changes. This cross-sectional analysis found that an evidence-based mental health intervention – the Common Elements Treatment Approach (CETA) - could positively impact chronic disease management. However, less costly mental health interventions may be worth exploring.
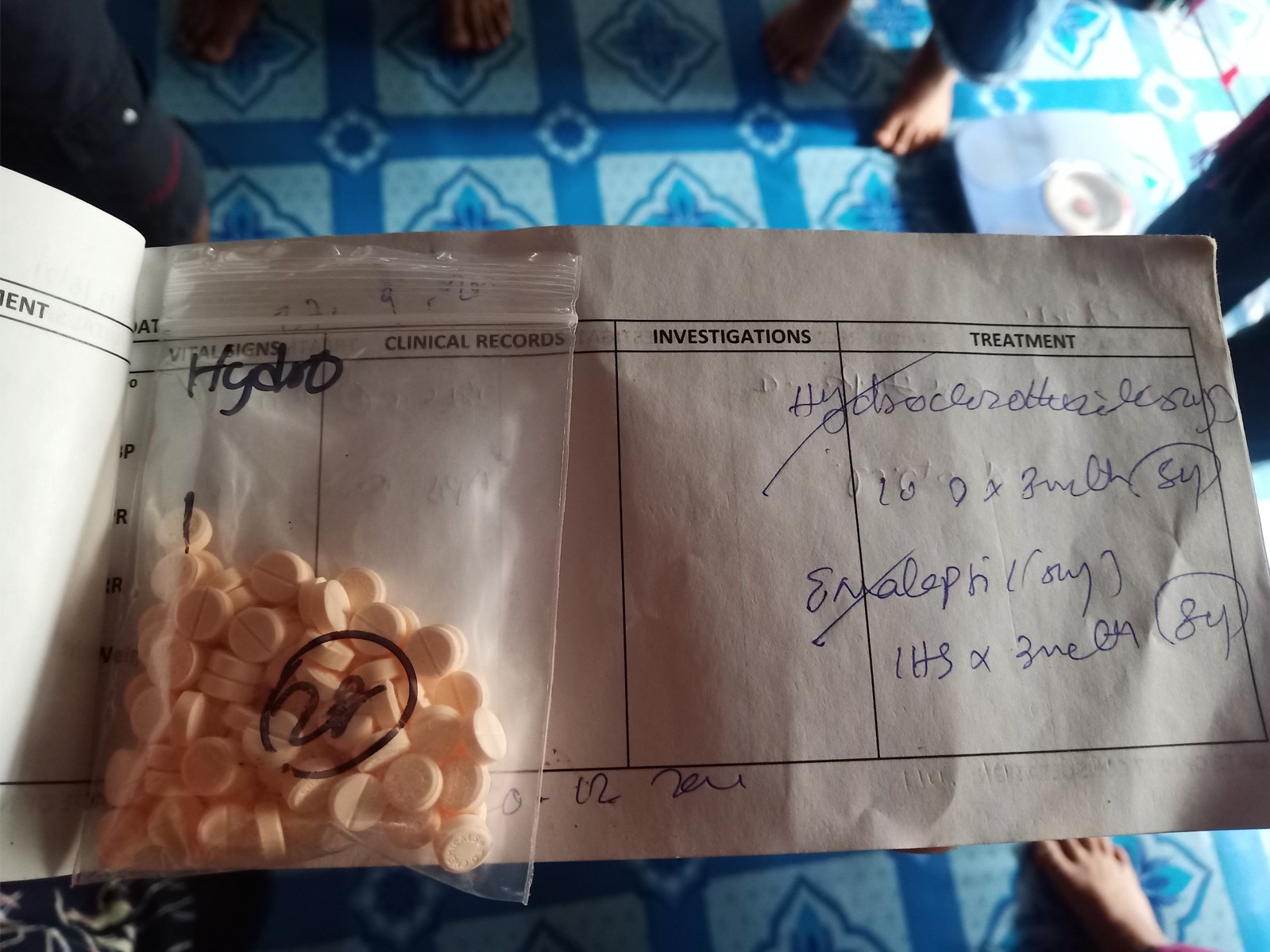
Poor mental health and treatment non - or poor - compliance have been linked among people living with chronic NCDs such as hypertension and diabetes mellitus. Treatment non-compliance compromises individual health and can increase healthcare costs. With the prevalence of NCDs rising among people affected by humanitarian crisis, as well as the increased risk of mental health conditions, evidence is needed on whether mental health interventions can address treatment non-compliance.
This research, which took place in a displaced persons camp in Thailand, explored whether the CETA intervention (a transdiagnostic mental health intervention designed for low resource settings) could positively impact chronic disease management. While positive impacts were found, including for self-reported medication adherence, more research is needed to explore the impacts on clinical outcomes and to optimise cost-effectiveness for varied contexts and patient groups. Targeted interventions for improving medication adherence could be a focus for future innovation.
This snapshot contains key messages, findings, implications for humanitarian policymakers and practitioners and recommendations for further research.
More information about this study can be found on the project profile.